Download the full brief
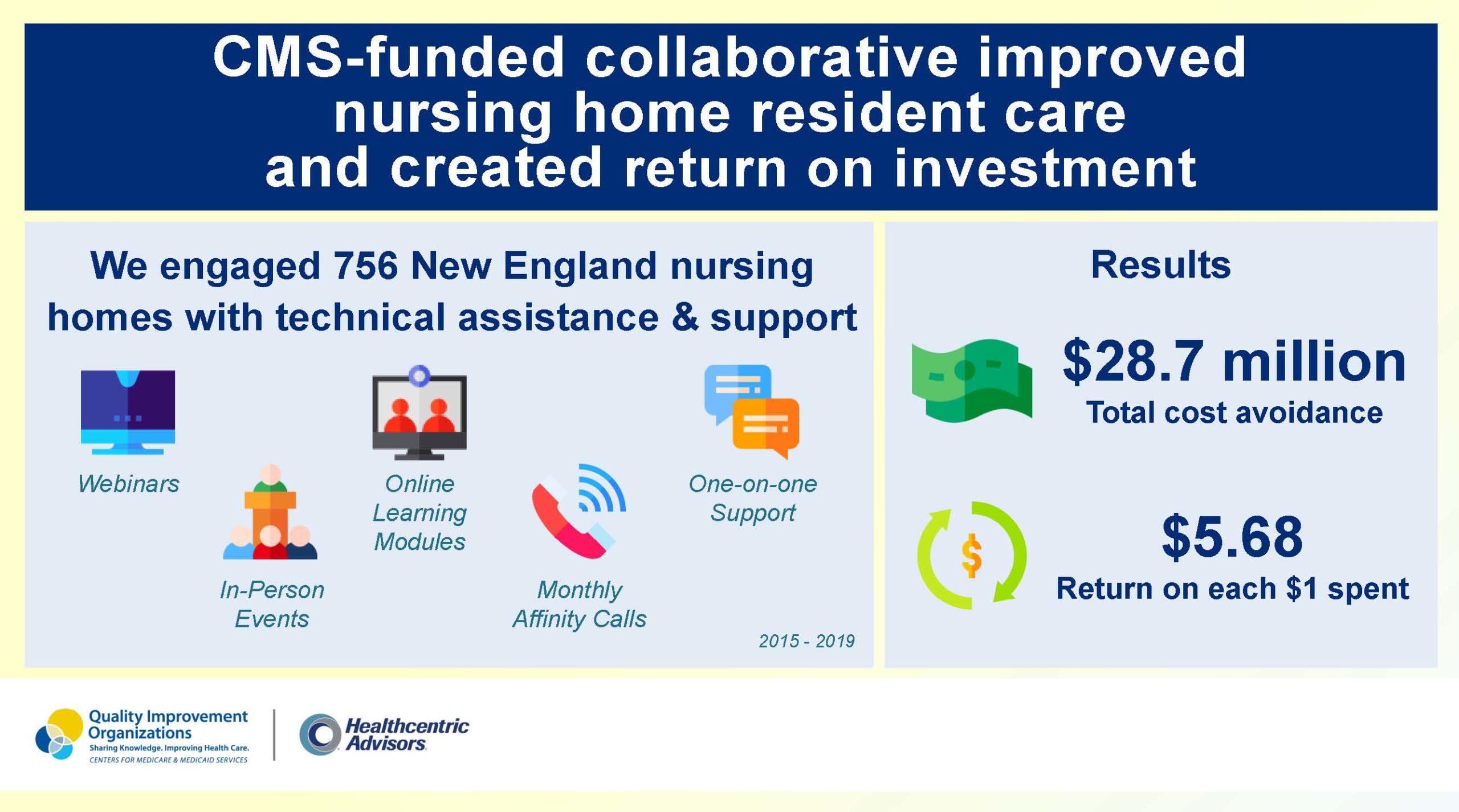
From 2015 to 2019, Healthcentric Advisors led the New England Nursing Home Quality Care Collaborative. Through the Collaborative, we engaged 756 nursing homes in all six New England states to help measurably improve the quality of care for their residents.
As part of the Centers for Medicare & Medicaid Services (CMS) Quality Innovation Network-Quality Improvement Organization (QIN-QIO) contract, this work included:
- Leading state coalitions
- Sharing facility quarterly reports
- Providing flexible education and support options to meet nursing home needs
- webinars and in-person events
- online learning modules
- monthly calls for affinity groups
- virtual and onsite technical assistance
- Encouraging overarching quality improvement strategies and addressing staff stability challenges
- Engaging with leadership at the facility’s corporate level to maintain communication and sustain efforts
Quality Measures of Focus
CMS tasked the Nursing Home Quality Care Collaborative with supporting improvement on 13 key quality measures. The following five measures were focus areas of education and support in New England and have clear cost associations based on existing literature:
- Percentage of long-stay residents who got an antipsychotic medication
- Percentage of long-stay low-risk residents who lose control of their bowels or bladder
- Percentage of long-stay residents with a urinary tract infection
- Percentage of long-stay high-risk residents with pressure ulcers
- Percentage of long-stay residents who lose too much weight
Return on Investment
Based on these measures, we calculated a total cost avoidance of $28,684,913 and a return on investment (ROI) of $5.68 per $1 spent by the funder, CMS, among the participating homes (Table). The total spending in 2017 dollars (7% discount rate) was $5,052,184. See the Methods section in the full report for further details.
Table. Costs avoided among the facilities participating in the Nursing Home Quality Care Collaborative (in 2017 dollars)
| Quality Measure | Annual Cost per Case | Cases Avoided 2016 |
Cases Avoided 2017 |
Cases Avoided 2018 |
Total Costs Avoided (7% discount rate) |
| Antipsychotic medication | $3,588 | 729 | 951 | 993 | $8,333,246 |
| Incontinence | $2,879 | -166 | -561 | -564 | -$3,182,825 |
| Urinary tract infection | $7,863 | 704 | 1,119 | 1,251 | $20,888,142 |
| Pressure ulcers | $4,425 | 178 | 276 | 190 | $2,489,155 |
| Weight loss | $89 | 676 | 925 | 400 | $157,194 |
| Total | $28,684,913 |
Implications
The ROI associated with improvement on key nursing home quality measures during the New England Nursing Home Quality Care Collaborative ($5.68 per $1 invested by the payer, CMS) demonstrates the value of investing in this work. Even if Healthcentric Advisors’ efforts only accounted for half of the quality measure cases avoided from 2016 to 2018, the ROI would still be almost $3 for every $1 spent. Therefore, investing in nursing home quality improvement through the QIN-QIO program in New England demonstrated improved care of nursing home residents, improved performance on nursing home quality measures, and avoided costs for CMS.